Despite the remarkable forward march of medicine, some treatments remain frustratingly stuck in the past. The treatment of abdominal aortic aneurysm – a bulge in the largest blood vessel that travels out from the heart – is a case in point.
Surgeons still follow guidelines established in the 1990s to treat aortic aneurysms. To balance the risks and benefits of surgical repair, the guidelines instruct surgeons to operate on aneurysms only if they are wider than 5cm (for women) or 5.5cm (for men). Surgeons may choose to operate on smaller aneurysms if they feel the patient is healthy enough to undergo surgery.
The decision is often a nail-biting one. While small aneurysms (under 5cm) are less likely to burst, they can still spontaneously rupture. If an aneurysm fails, the chance of death is upwards of 90%. However, aneurysm repair also carries risks, including bleeding, infections, and other complications.
“It’s a bit absurd to think that you have a patient that has a known aneurysm in their abdomen. The surgeon says, ‘Look, we’re going to call you back for another scan in a year, and we’ll see if it has grown, but these patients know there’s a risk their aneurysm could rupture at any time. In fact, the risk of a small aneurysm rupturing is 1-in-8.’” explains Dr. Mitchel Benovoy, CEO of ViTAA Medical.
Using AI-assisted 3D modelling, ViTAA Medical is determined to bring aneurysm management into the 21st century. For the last 15 years, Dr. Elena Di Martino, a biomedical engineer and Dr. Randy Moore, a vascular surgeon (both teach at the University of Calgary), have been perfecting technology that uses computer algorithms to analyze information gathered on a CT scan to create 3D models of aneurysms that encode the actual mechanical properties of the vessel’s wall. The final model the surgeon uses is a gradient colour scheme to illustrate the weakness and strength of the vascular tissue.
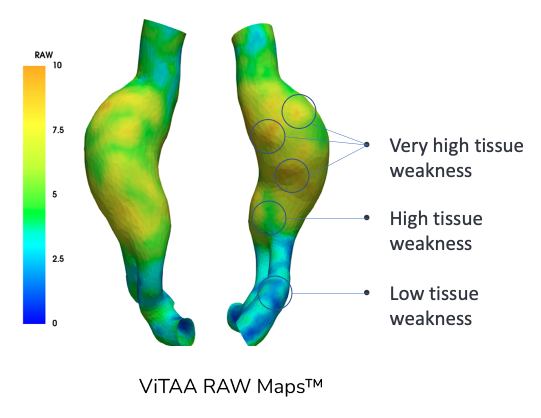
The tool also calculates a risk score for aneurysms between 0 to 10, with 0 indicating “very strong and healthy tissue, and 10 being extremely degraded and weak tissue not unlike tissue paper” explains Benovoy. As one can imagine, aneurysms with strong vascular walls are less likely to burst than those as fragile as mushy paper.
The ViTAA score is based on three different factors. One is the blood flow patterns in the aneurysm, which shows how much shear stress the flow is placing on the vessel walls. Benovoy likens this to “the effect of the ocean waves gradually eroding the shoreline.” Another is how the aneurysm changes shape when blood pulses through it. For example, weak spots in the aneurysm will expand more when blood flows into it, compared to stronger areas. The score also accounts for the thickness of the blood clot that forms within the aneurysm, which creates a low-oxygen and inflammatory bed that contributes to the degradation of the structure of the vessel walls.
While the 3D map and score are far more useful than the crude diameter measurement that most surgeons today use to decide on surgery, the ViTAA Medical team wanted to make the decision even clearer. Using funding from INOVAIT, the company developed and trained an AI framework to explain itself. The ViTAA team knew it would be important for the physicians to understand how the AI reached its conclusions. ViTAA calls their AI program a ‘glassbox’, which contrasts other commercial AI models that are opaque – blackboxes. Every step and decision their AI system takes is fully auditable and easily understood by physicians. The team knew their proprietary biomarkers were as strong as their AI models and quickly learned to predict which patients’ aneurysms went on to grow and whether or not they would rupture with astounding accuracy.
A study published in 2023 demonstrated that their AI model accurately identified which aneurysms would grow at an accelerated rate in the next 12 months. Then, in 2024, ViTAA Medical presented their latest data showing “the holy grail,” as Benovoy puts it – that their AI system could predict which aneurysms would rupture. The model had a sensitivity of 100% and a specificity of 92%. That means that every aneurysm the AI system predicted would rupture had in fact ruptured, while 8% of aneurysms the AI model predicted would not rupture had, in fact, burst. (The AI model analyzed historical data, so the outcomes are known). The model assessed aortic abdominal aneurysms between 4.6cm and 12cm.
ViTAA Medical doesn’t only want to improve the identification of patients who need aneurysm repair surgery but also those who don’t require surgery. The company also wants to improve the surgery itself.
To repair an aneurysm, surgeons place a stent (a tube) in the blood vessel so that the blood flows through the stent rather than the weakened part of the blood vessel. However, surgeons can place the stent in weak tissue, which can later lead to blood trickling between the stent and the vascular wall. This can cause a post-surgical rupture, and it’s the reason aortic aneurysm repair has very high complication rate.
But by mapping tissue weakness and strength in the blood vessel, the ViTAA software directs surgeons to anchor the stent in strong, rather than weak, tissue. This can dramatically reduce the risk of post-surgical complications. ViTAA Medical is currently running clinical trials to evaluate the outcomes of patients whose aneurysms will be planned with ViTAA’s tissue strength technology and those whose aneurysms were repaired without the tool.
Vascular surgeons can see the transformative potential of ViTAA Medical-image-guided surgery. Representatives of the Society of Vascular Surgery in the U.S. recently approached ViTAA Medical, offering to fully endorse the technology.
ViTAA received their first FDA approval in November, which means the technology can be used on a daily basis in the clinical management of patients with aneurysms. In the coming years, ViTAA Medical plans to adapt its technology for diagnosing and treating aneurysms elsewhere in the body, including in the chest and brain.
Early funding from INOVAIT enabled ViTAA Medical to fund its AI prediction research. “Thanks to INOVAIT, we were able to prove to other investors that our technology is transformational,” says Benovoy.
Learn more about ViTAA Medical’s INOVAIT Project here.
In the meantime, Benovoy is confident that ViTAA Medical’s tool can save lives. Recently, a doctor described a case where they sent the patient’s data to the company. The ViTAA technology showed illustrated “two bright red spots,” suggesting extremely weak tissue. Then during surgery, the surgeon lightly pushed on the spots that was showing up as a hot zone. His finger went through the tissue. “The doctor told us he had an Aha-moment at that point,” says Benovoy. The aneurysm was so weak that it could have burst from the patient simply bending down to pick up something.
Every year, some patients die when their aneurysm bursts spontaneously, between appointments to monitor the size. “Frankly, the surgeons hate this reality,” Benovoy says.
With ViTAA Medical, surgeons will no longer assess aortic aneurysms on size alone. Instead, they’ll factor in multiple markers of vascular tissue strength and AI prediction. In Benovoy’s mind, there’s no doubt. “This technology saves lives.”